Sree Chaguturu is CVS Health’s senior vice president and chief medical officer for CVS Caremark.
As the United States grappled with the enormous threat posed by the coronavirus last spring and social distancing measures took hold, we saw a significant drop in people accessing routine and preventive care. With a new, deadly and little understood virus, many healthcare providers shut down for non-emergency medical care.
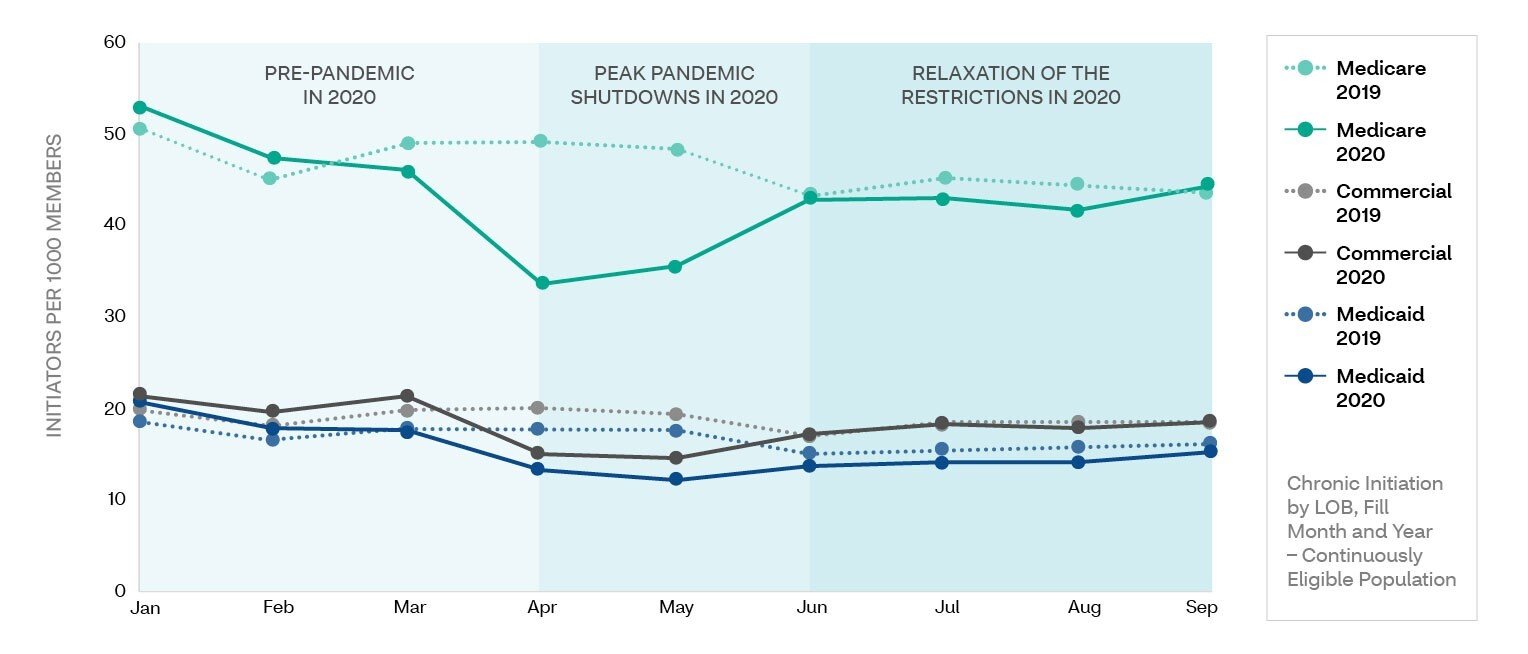
To better understand the impact of the pandemic on access to needed medications, my team at CVS Caremark analyzed prescription claims data from the peak of shutdowns in spring 2020 through the relaxation of restrictions in the fall. For our analysis, we focused on those either initiating treatment for common chronic health conditions, or adding new treatments to their existing regimen.
As we reported in the 2020 CVS Caremark Drug Trend Report, we found a steep drop-off across the board in people accessing medications, with a reversal — although not to pre-pandemic levels — when restrictions began to be relaxed in the third quarter. While the findings confirmed what we expected, they also revealed a concerning pattern that reinforces the impact of — and the need to address — social determinants of health.
Permission granted by CVS Health
The drop in utilization was highest in the Medicaid population and the recovery, smallest. Medicaid patients are generally from lower-income households and often from more vulnerable populations including rural communities and people of color who already face significant health disparities. And, chronic conditions like heart disease, hypertension, hyperlipidemia and diabetes are highly prevalent amongst Medicaid recipients. While the data does not show a direct correlation, it is possible — even likely — that at least some of those who stopped seeking care at the height of the pandemic and did not resume later in the year within the Medicare and commercial populations are also those who are most likely to experience health disparities linked to social determinants of health like limited access transportation and proximity to a pharmacy.
This means potentially millions of Americans are not seeking or receiving the care they need for serious chronic conditions because of disruptions from the COVID-19 pandemic. This disparity not only puts individuals at significant risk, it can also have an impact on our entire healthcare system because untreated and undertreated chronic diseases can lead to health complications resulting in disease progression, hospital stays, and other comorbidities that strain limited resources.
As vaccination rates climb and we enter what is hopefully the end stage of the COVID-19 crisis, we must make sure that we do not allow the rise of untreated chronic illness to become an even greater side-effect of the pandemic — especially for those who already face challenges interacting with the healthcare system. The good news is that we have the tools to tackle this challenge and ensure that those at risk of chronic diseases receive the right interventions at the right time. In order to ensure that the challenges of the COVID-19 pandemic do not result in less or worse care in these communities, the healthcare industry must:
Engage with patients in vulnerable communities more often, being responsive to the needs and the challenges they are likely to face. This means rethinking how we communicate health risks and using channels that each individual is more likely to respond to — for instance, text messages instead of email or phone work better for certain people and demographic groups.
As much as the medium matters, so does the message — we need to address and overcome language and communications barriers to ensure that people are not only aware of their health risks but equipped with information about how and where they can get support that works for their lifestyle, economic situation and health needs.
In addition to tackling the challenges of communication about disease risk, we must provide support and treatment options that work for, and with, those who are at the highest risk. This means more personalized, tailored screening and treatment options that take into account individual health histories as well as demographic patterns based on age, gender, education level, geography, income and race. For instance, providing screenings and care for conditions like diabetes or heart disease at locations that are accessible to people who have rigid work schedules or transportation challenges and offering affordable access to telemedicine and remote monitoring that can make it easier to track chronic disease and adhere to treatments.
We must commit to working within the communities that face health disparities to address the things that have often driven or increased those disparities — affordability, accessibility, awareness and trust. We can do this by engaging with community leaders, nonprofit and faith-based organizations, and other familiar and trusted local pillars to communicate health messages and improve access to health services.
We have a responsibility to ensure that the immediate health impact of the virus doesn’t exacerbate existing health challenges like the fight against chronic disease and systemic health equity gaps. By carefully monitoring utilization patterns and demographic trends, we can identify the spillover effects from the pandemic. But we must take additional steps to address these trends and ensure that no one — especially those already impacted by healthcare disparities — lacks the care and support they need.
Looking ahead, data and analytics will play a key role in reducing health disparities and supporting chronic disease management.
Moving from simply understanding that care gaps exist to using data to pinpoint ways to close them will be critical in tackling the challenges of health disparities and chronic disease.
