Recently, I discussed the dirty secret of the SSRI antidepressants — they cause psychotic violence which typically results in suicide and sometimes in horrific homicide (e.g., mass shootings). Remarkably, this side effect was discovered in their clinical trials, covered up by the drug companies, and then covered up by the FDA after the agency received a deluge of complaints (39,000 in the first nine years) once the first SSRI, Prozac, hit the market.
However, since that psychotic violence is such a distinct and alarming side effect, it motivated many of the families of those who died to sue those drug companies and get proof the pharmaceutical industry had indeed covered this up to protect the sales of their lucrative antidepressants.
As a result (because of the discovery process), we have a much clearer picture of what actually happened with the SSRIs than many of the other terrible pharmaceuticals on the market.
Note: In addition to being quite dangerous, SSRIs do not benefit the majority of patients who receive them (which makes it incredibly difficult to justify pushing these drugs). It is thus a great tragedy the need to “treat depression” with these bad drugs has been so effectively marketed to the world, while numerous safe and effective treatments for depression (discussed in the latter part of this article) have been ignored (as no one can make money from them).
Sadly, this is a common pattern you observe within the medical industry, best illustrated by numerous effective but off-patent treatments for COVID-19 being blacklisted while numerous unsafe and ineffective therapies were pushed on the world.
The Toxicology Bell Curve
In toxicology, you will typically see severe and extreme reactions occur much less frequently than moderate reactions:

Because of this, when a very concerning and unmistakable adverse reaction occurs (e.g., the COVID-19 vaccines causing sudden deaths in young healthy athletes) that suggests you are seeing the tip of the iceberg and far less severe injuries are also occurring much more frequently.
For example, one estimate found that of those vaccinated, 18% were injured, 0.93% were disabled, and 0.05-0.1% died, and another survey found 41% of those vaccinated were injured, with 7% being severely injured.
Note: Since you can’t survey someone who is dead, that survey company did the next closest thing and found 24% to 28% of people know someone they believed died from the COVID vaccine.
In the case of the SSRIs, the psychotic violence they can create is just the visible tip of the iceberg, and there are many less severe but still awful ways they warp your mind. For example, in a survey of 1,829 patients on antidepressants in New Zealand, 62% reported sexual difficulties, 60% felt emotionally numb, 52% felt not like themselves, 39% cared less about others, 47% had experienced agitation and 39% had experienced suicidal ideation.
Note: Other less common reported side effects (in order of decreasing frequency) in that survey included: insomnia, nightmares, ‘Fuzzy’/‘zombie,’ jaw grinding, sweating, blurred vision, constipation, disturbed/restless sleep, anxiety, heart palpitations, difficulty thinking, fatigue/exhaustion, strange/vivid dreams, stiff muscles/joints, ‘Brain zaps,’ mania, excessive yawning, panic attacks, memory loss, decreased motivation, night sweats, decreased appetite.
This list matches what I’ve seen in many similar assessments (although others like feeling agitated, shaky or anxious, indigestion, stomach aches and diarrhea are also commonly reported).
Most importantly, the respondents to that survey reported that their prescribers did not warn them about many of these side effects (e.g., the emotional numbness or their interactions with other people). As many people I know have been severely impacted by these drugs and gaslighted by the doctors they sought care from, especially when they dealt with one of the most challenging aspects of these addictive drugs — how you get off them?
General Problems With SSRIs
Note: Most of the issues described through this article apply to SSRIs and SNRIs. For ease of reading, I will just refer to SSRIs. Likewise, in some cases, “antidepressants” sometimes also refers to other classes of drugs (e.g., tricyclics).
One of the lesser known facts about the pharmaceutical industry is that more money is spent marketing drugs than developing them (this was even the case during COVID when the industry had been given a virtual monopoly because the government suppressed every off-patent medication).
In turn, you will frequently observe the industry concoct elaborate ways to make a useless (or worse) drug appear to be worth selling to all of America (in my opinion best encapsulated by the idiom “Putting Lipstick on a Pig“).
This I believe occurs because clinical trials cost so much to do and the company needs to guarantee a return on that investment. It is also because the drug regulators (who often are taking money from the industry) never hold them accountable for that behavior.
Note: Numerous whistleblowers testified that the COVID-19 vaccine trials were conducted in a fraudulent manner which deliberately overestimated the efficacy of the vaccines and concealed those who were severely injured by them. Despite this (even after receiving a formal complaint from a researcher at one Pfizer trial site), the FDA refused to do anything.
Since “depression” is so subjective, it is even easier to game its research, and as a result, when the “successful” studies of antidepressants are carefully examined, we find over and over that they actually provided minimal benefit to the recipients but severely harmed many of the test subjects (in essence exactly what happened with the COVID-19 vaccines and their predecessors, the disastrous HPV vaccines).
Fortunately, there are a few metrics you cannot cover up. One of the most well-known ones is overall mortality (how many people in total on vs. off the drug died) since you can’t reclassify death, and by this metric, the “life-saving” COVID vaccines for example failed to live up to their promise. Another is how many patients voluntarily chose to continue taking a medication:
- A review of 29 published and 11 unpublished clinical trials containing 3704 patients who received Paxil and 2687 who received a placebo, an equal proportion of patients in both groups left their study early (suggesting Paxil’s benefits did not outweigh its side effect), and that compared to placebo, 77% more stopped the drug because of side effects and 155% more stopped because they experienced suicidal tendencies.
- A study of 7525 patients, found that 56% of them chose to stop taking an SSRI within 4 months of being prescribed it.
- An international survey of 3,516 people from 14 patient advocacy groups found that 44% had permanently stopped taking a psychiatric drug due to its side effects.
- A survey of 500 patients found 81.5% were unsure if their anti-depressants were necessary.
Put differently, if patients feel worse on a medication they are taking to “feel good” then you do without it, that means the trials proclaiming the medications made patients feel better were a fraud.
Unfortunately, since there is so much money in the psych meds (as you can sell those pills indefinitely to as much of the population as you can give a “diagnosis” to), there is a vested interest to not reveal those side effects or provide resources for those suffer from them (as doing so would effectively be an admission to those side effects existed).
This in turn becomes particularly problematic when the patient develops a severe acute reaction (e.g., the psychosis that can turn violent), a permanently debilitating chronic reaction, or severe withdrawals when they try to stop using these highly addictive drugs.
“When people read other people’s stories, they realize that they’re not the only person that’s experiencing that problem. There are 6,000 relatively complete case histories [on SurvivingAntidepressants.org]. You realize it’s all the same story. It’s one story.
And each person who experiences it is so surprised that it happened to them — people go through a period of absolute disbelief. They realize that they’ve been trusting their doctors to have a certain amount of knowledge, and their doctors don’t actually have that knowledge.
And you know, this is heartbreaking. I went through this, and I felt that the world had fallen out from underneath me. There wasn’t any medical safety net. So the sociological phenomenon exists, and has not yet filtered into medicine [this is also exactly what has happened with the COVID-19 vaccines].
Medicine has its own ways of gathering information, and in psychiatry, for some reason, they keep asking each other what the truth is instead of asking their patients. The patient voice is not very well recognized in psychiatry at all.”
Note: Surviving Antidepressants is a popular website (with 500,000 views a month and 14,000 users from every imaginable demographic) that the founder was forced to make because no resources existed for those with SSRI complications. In the above interview, she highlights another common issue SSRI victims face.
Because there is so much stigma towards mental illness, when a “psych patient” shares their reaction to a medication, it is often discounted and attributed to their existing mental illness rather than the drug and is “treated” by giving more of the drug — which often has disastrous consequences (e.g., this is a common story with the mass shooters).
Violent Behavior
When Prozac was first brought to market in the mid-1980s, the pharmaceutical industry had not yet convinced the world everyone was depressed and needed an antidepressant. So, instead (given that SSRIs work in a similar manner to a stimulant like Cocaine) Prozac was initially marketed as a “mood-lifter.”
Likewise, in 1985 when the FDA’s safety reviewer scrutinized Eli Lily’s Prozac application, they realized Lily had “failed” to report psychotic episodes of people on the drug and that Prozac’s adverse effects resembled that of a stimulant drug.
In turn, the warnings on the labels for SSRIs, such as anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia, hypomania, and mania match the effects commonly observed with stimulant street drugs such as cocaine and methamphetamine.
Note: In the previously mentioned survey of 3,516 people which found 44% stopped a psych med due to side effects, a quarter reported this was due to the agitation they suffered.
In the previous article, I published a variety of studies showing that the manufacturers knew this violent behavior (e.g., suicide) was a common side effect of the SSRIs that was deliberately kept from the public. Since a common argument used to debunk that assertion is claiming that this behavior was actually due to a pre-existing mental disorder, I would like to cite three studies which disprove this notion:
• A Cochrane review assessed 150 studies where healthy volunteers were given SSRIs, and found approximately one third of them deliberately omitted discussing SSRI side effects and about half of the studies were never made publicly available (presumably to hide their concerning data).
Ultimately, 14 of the 150 studies were eligible for meta-analysis (since enough information existed in them for the researchers to know what actually happened), and in these 14 studies, SSRIs were found to double the risk of suicide.
• In 2000, David Healy published a study he had carried out with 20 healthy volunteers – all with no history of depression or other mental illness – and to his big surprise two (10%) of them became suicidal when they received Zoloft. One of them was on her way out the door to kill herself in front of a train or a car when a phone call saved her. Both volunteers remained disturbed several months later and seriously questioned the stability of their personalities.
• Eli Lilly showed in 1978 that cats who had been friendly for years began to growl and hiss on Prozac and became distinctly unfriendly. Once Prozac was stopped, the cats returned to their usual friendly behavior in a week or two.
Note: The FDA hypothesized that SSRIs can reduce violence in some but cause an increase in violence in others (which I suspect is linked to pre-existing genetic polymorphisms — as hypomethylators respond well to SSRIs whereas hypermethylators can turn violent on them).
Likewise a review of 84 animal studies showed that reduced aggression upon treatment with SSRI was most commonly observed, but sometimes the animals instead became more aggressive.
To illustrate what this can look like, I will share what four different patients experienced prior to killing themselves or others:
“A month later, Toran experienced a severe cluster of adverse reactions including suicidal behavior, self-harm, aggression, hostility, hallucinations, lack of concentration and impaired functioning. The symptoms were so severe that he dropped out of school. His psychiatrist’s response was to increase his dose, which worsened the adverse reactions.
Six days later, Jake had his first reaction. He walked out of an exam half-way through it and cried for about 2-3 hours that night, saying, ‘You don’t know what it’s like in my head.’ His parents thought this was from the stress of the exams. They never imagined that a drug could do this to a person.
The last two days she was just a complete zombie I have to say. She was just agitated, jumping at every noise and not making sense. I was very concerned. We were very close to Cecily. I just loved her deeply.
Shortly before his death, Woody came home crying after driving around all day. He sat in a fetal position on the kitchen floor profusely sweating with his hands pressing around his head saying, ‘Help me. Help me. I don’t know what’s happening to me. I am losing my mind. It’s like my head is outside my body looking in.'”
While these cases are extreme, I know numerous people who had less extreme versions of the above (e.g., they never committed a violent act). Each of them shared with me just how terrifying it was for them to gradually lose their mind or that their brain just never worked right after SSRIs, and I hope this article can provide an inkling of what it’s like to go through that.
Bipolar Disorder
Since the SSRIs antidepressants are stimulants they often trigger mania, and in turn, one of the most common problems associated with their use is bipolar disorder (a disease where you alternate from a depressed to manic state). To put this into context, in 1955, 1 in 13,000 people were disabled for bipolar and the majority of patients who presented to the hospital for a manic episode permanently recovered.
Now, bipolar affects 1 in every 20-50 people and 83% of them are severe impaired in some facet of their lives. A significant amount of data has linked bipolar disorder to SSRIs. For example:
• Yale researchers reviewed the records of 87,290 patients diagnosed with depression or anxiety between 1997 and 2001 and determined those treated with antidepressants converted to bipolar at the rate of 7.7 percent per year (three times greater than the rate for those not exposed to the drugs), ultimately resulting in between 20 to 40 depressed patients becoming bipolar.
• A survey found 60% of bipolar patients only developed their illness after receiving SSRIs for depression.
• Peter Breggin reported that of 184 patients in hospital starting Prozac, Zoloft or Paxil, 11 developed mania and 8 became psychotic, and in Yale, 8% of 533 consecutive admissions were for mania or psychosis caused by antidepressants, and two patients heard voices commanding them to kill themselves.
Note: The psychiatric field gets around this issue by claiming SSRIs “unmask” latent bipolar a patient always had — even though it likely would have never been “unmasked” had they never taken the SSRI in the first place.
Likewise, since the advent of mass psychiatric medicating, the character of bipolar has changed, becoming much harder to treat, characterized by much more rapid cycling between the depressed and manic states and much more likely to produce severe complications like dementia later on.
Unfortunately, when the foremost experts in bipolar disorder presented these findings at the American Psychiatric Association’s annual conference and urged caution in the over administration of SSRIs, they were met with boos from their increasingly upset audience.
Note: A strong case can be made that many of the disastrous complications of bipolar disorder result from the highly toxic antipsychotics the disorder is “treated” with, especially since those same drugs are often given to schizophrenic patients, a disorder characterized by similar long term complications (that are rarely seen in countries which do not use the drugs).
Unfortunately, doctors instead are typically taught to see the severe long term consequences associated with those disorders as a justification for why it is critical to “treat” the disorders, rather than to reconsider drugging their patients (which is often the actual cause of those consequences).
Sexual Dysfunction
One of the side effects that I feel best illustrates the actual risk/reward ratio of the SSRIs is sexual dysfunction — as not being able to have sex is quite likely to make someone depressed (and as Gøtzsche shared, in some cases suicidal), hence often completely invalidating the justification for taking a SSRI to “feel happy again.”
For example, a Spanish study of five of the most commonly prescribed SSRIs found on average that the drugs caused sexual disturbances in 59% of 1,022 patients (who all had a normal sex life before they started on drug), and 40% of the 1,022 considered that dysfunction unacceptable. When Peter Gøtzsche looked at each of those side-effects he found:
- 57% experienced decreased libido
- 57% experienced delayed orgasm or ejaculation
- 46% experienced no orgasm or ejaculation
- 31% experienced erectile dysfunction or decreased vaginal lubrication
Note: Similar results have been obtained in other studies and I know numerous male and female patients who continued to experience sexual dysfunction long after they stopped the SSRI.
What I find the most amazing about this side effect is that while the psychiatrists tends to downplay or ignore it, they simultaneously market SSRIs to treat premature ejaculation — which is yet another example of the drug industry trying to have its cake and eat it (especially given that many of the SSRI manufacturers also sell drugs for erectile dysfunction).
Note: One reason this side effect is under recognized is because embarrassed patients often won’t report it unless they are specifically asked about it (e.g., in the Spanish study, while 59% of SSRI users reported sexual dysfunction, only 20% do so without prompting — something unlikely to be done by a drug trial aimed at getting a medication to market).
Emotional Anesthesia
At the time the SSRIs began to be approved, I was not yet begun studying the regulatory process in detail, so I did not notice their issues until I started seeing them around me. The first and foremost thing I noticed was that the SSRIs dramatically altered the personality of those who took them, and often sedated a lot of people who previously had the drive to make something of their life — and in some cases, I sadly watched that derailment continue for decades.
In time, I began to hear stories of people describing how their experience of life was deadened, often in a manner not too different from how the drugs “numb” your sexuality. Some of the common stories included:
• Not having emotional responses to things you should have responses to — For example, I heard numerous cases of people being in unhealthy jobs or relationships, seeing a doctor for help with their depression, quickly being put on Prozac, and then wasting a decade of their life because Prozac removed their drive to leave that situation. Likewise, I heard many people state that Prozac took away the joy they felt in life.
• Losing the depth and richness of life — This comment does an excellent job of illustrating the phenomenon:
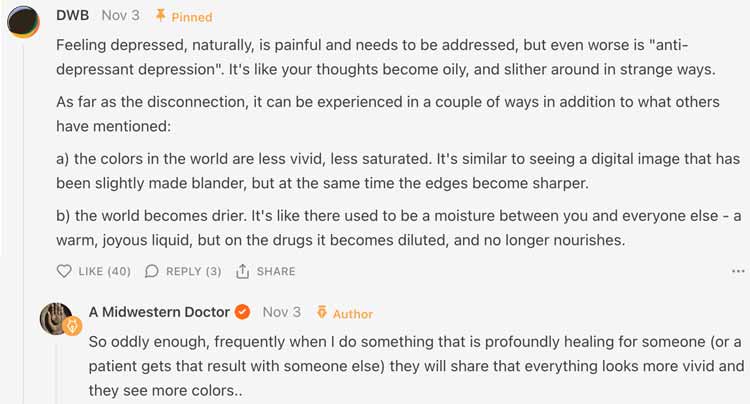
In the psychiatry, this experience (e.g., not finding things as enjoyable as they used to) is known as “emotional blunting,” although I and others believe “emotional anesthesia” is a more accurate depiction. Depending on the study (e.g., those mentioned above) between 40-60% of those who take SSRIs experience this side effect and it’s sometimes rationalized as a necessary trade-off for removing the emotional pain associated with depression.
In my eyes, one of the greatest problems with our society is the belief our media has marketed to us that we should never have to feel negative emotions. In reality, they are a critical component of the human experience and are frequently necessary for us our growth and identifying the correct direction for our life.
Birth Defects
Once a drug gets approved, pharmaceutical companies will always try to expand their market for it (e.g., this is why after adults stopped wanting the initial COVID-19 vaccine everyone pivoted to mandating them on children — even though children have an almost 0% chance of dying from COVID-19).
With SSRIs, the industry has likewise worked to push them on vulnerable groups (e.g., foster children, “struggling” students, prisoners or parolees, pregnant mothers and the elderly) and each group has suffered significant consequences from these practices. This excellent skit by Peter Gøtzsche illustrates the absurdity of pushing them on pregnant women:
Pushing SSRIs on pregnant women is rationalized by the fact women frequently get depressed during or after their pregnancies (which is often due to excessive copper levels — something quite easy to treat naturally). Unfortunately, there are a variety of reasons why SSRIs are not safe during pregnancy. These include:
• SSRIs increases the risk of premature births, with the greatest risk (a doubling) occurring if an SSRI is taken during the third trimester.
• SSRIs significantly increase the risk of septal defects (which often require heart surgery to repair). For example, a study of 500,000 infants in Denmark found mothers taking a single SSRI while pregnant caused the likelihood of a septal defect in their child to go from 0.5% to 0.9% and taking two or more increased it to 2.1%.
Additionally, while on average taking an SSRI doubled the risk of a birth defect, the increased risk ranged from 34% to 225% depending on the SSRI.
Note: A popular weight-loss drug, Fen-Phen, which worked by spiking serotonin levels in the body was withdrawn from the market after it caused many cases of deadly heart valve defects and pulmonary hypertension (along with 30% of the recipients developing an abnormal echocardiogram).
• SSRIs significantly increase the risk of persistent pulmonary hypertension in a newborn baby. One study of 1173 babies found SSRIs increased the risk of it by 6.1 times, while another found the risk increased by 4.29 times, while another found it increased by 2.5 times.
Given that this condition affects 1-2 out of 1000 births and is often fatal, this “small” risk adds up quite quickly (but nonetheless this was not enough for the FDA to reconsider its advocacy of these drugs for pregnant women).
Note: Other newborn complications linked to SSRIs include irritability, tremor, hypertonia and difficulty sleeping or breast feeding.
Sadly, after birth SSRIs continue to affect the development of a child. For example the package insert for Prozac states that after only 19 weeks of treatment, children had lost 1.1 cm (0.43 inches) and 1.1 kg in weight (2.43 lbs) compared to children treated with placebo.
Likewise, many members of the surviving antidepressants community have observed a large number of chronic health issues (e.g., gastrointestinal, endocrine or autoimmune) that appear to follow long term use of an SSRIs, and then often slowly improve once the drugs are discontinued. Unfortunately, data in this area is much more limited (as there is minimal motivation to study it).
Withdrawals
One of the nastiest issue with the SSRIs they are often extremely difficult to stop using, and frequently, that addiction can start after a very brief course of the SSRI (e.g., a month).
Sadly, when patients suffer SSRI withdrawals doctors typically interpret it as relapse and a sign the withdrawn medication was “working” (hence needing to be resumed) or recognize it is in fact a withdrawal, but only know to “treat” it by resuming the addictive drug.
Note: This is somewhat analogous to the COVID-19 vaccines as the “immunity” they provide rapidly wanes (in the course of a few months), at which point one becomes more likely to get COVID than if they had never been vaccinated (especially after multiple vaccinations).
This in turn was why many health authorities recommended more and boosters even though that inevitably could not lead to a good outcome, best illustrated by so many vaccinated people who keep getting COVID but are somehow grateful to have been vaccinated because the vaccine “protected them from it being worse.”
When the withdrawals occur, they can often trigger psychotic violence, and sadder still, those same changes can be triggered simply by changing the dose of a SSRI (by increasing or decreasing it), or changing to another SSRI (which sadly is a common story in many of the SSRI homicides or suicides). Likewise, less severe (and often fluctuating) symptoms also occur such as:
- The feeling of an electric shock in your arms, legs, or head (these horrible things are commonly referred to as “brain zaps” and have happened to so many people I know)
- Dizziness (mild to severe)
- Visual problems
- A large number of sensitivities (e.g., to light, heat, a supplement or food)
- Anxiety which comes and goes, sometimes in intense ‘surges’
- Difficulty in getting to sleep and vivid or frightening dreams
- Low mood, feeling unable to be interested in or enjoy things
- A sense of being physically unwell
- Rapidly changing moods (e.g., spontaneous weeping spells, attacks of sheer terror, or sudden plunges into unprecedented contentless black holes of pure dread).
- Anger, sleeplessness, tiredness, loss of co-ordination and headache
- A feeling that things are not real (‘derealisation’), or a feeling that you have ‘cotton wool in your head’
- Difficulty in concentrating
- Suicidal thoughts
- Queasiness or indigestion
- A feeling of inner restlessness and inability to stay still (this is known as akathisia and often preceeds psychotic SSRI violence)
- Crippling muscle pain or spasms
Furthermore, these reactions are very common. A recent meta-analysis found that 56% of patients who stop using SSRIs experience withdrawals, that 46% who stop an SSRI experience severe withdrawals, and that these withdrawals last for weeks to months. Additionally, it is well known in the SSRI recovery community that the risk of a withdrawal varies greatly depending on the drug (Paxil is notorious for this, Cymbalta is also a common offender).
Note: A 1996 door to door survey of 2003 randomly selected people in England found that 78% of them considered SSRIs to be addictive.
The industry is well aware of this, to the point they will often deliberately put “placebo” subjects in SSRI trials into withdrawals (by terminating their existing prescription) so they can make the drug group look “better” than the “placebo” patients.
Note: This is similar to how for the Gardasil HPV vaccine, to “hide” it’s extraordinarily high rate of adverse reactions (e.g. autoimmune ones) Merck chose to have its “placebo” group receive the highly toxic adjuvant also used in Gardasil. As a result, similar injury rates occurred in both groups, but no regulator ever questioned why the baseline injury rate was so high to begin with.
Quitting SSRIs
For the roughly 50% of people who experience SSRI withdrawals, one of the most challenging things is how incredibly slowly they have to stop taking them. A major reason for this is due to the non-linear relationship between an SSRI dose and its binding to the brain (e.g., its striatum).

Note: The above graphs were sourced from this study. Additional ones can be found in this post.
What the above graph essentially means is that:
• To reduce a SSRI, you have to also match that curve, which requires decreasing your dose by a progressively slower rate (once a month reducing last months dose by 10% is commonly recommended).
• This process thus often takes a long time (e.g., people often stop at 2.5% of their original dose, which requires reducing the dose by 10% thirty-five times).
Note: In the best case scenario, they find antidepressant can be withdrawn from in 6 months. Typically it takes years.
• SSRIs are given at a much higher dose than appropriate (hence making them extremely addictive).
Note: Incorrect dosing is an extremely common problem in standardized medicine and was discussed further here.
• Since, at most, people can tolerate withdrawing from one SSRI (or antipsychotic) at a time, the withdrawal process becomes much more challenging when patients are on multiple drugs (which sadly is very common in psychiatry).
Note: Paxil is particularly difficult to withdraw from because it inhibits its own metabolism, so as you lower the dose of it, it gets metabolized faster and you become more likely to suffer withdrawals. Additionally, Paxil can cause alcohol cravings and lower ones resistance to those cravings (which, as discussed below, can become a huge problem).
When SSRIs were discovered, the industry created the mythology that they worked by fixing a serotonin deficiency in the brain. As the years went by, that was gradually disproven, and the field eventually concluded they instead worked by rewiring your brain (which is why psychiatrists tell you to keep taking an SSRI even if it doesn’t initially work as they want a few weeks for that “beneficial” rewiring to take place).
So, to “cure” an SSRI addiction, you need to let the brain rewire itself back to normal, and until that happens, the brain will behave in an abnormal fashion (e.g., its ability to adapt to outside stressors in a healthy way is dramatically reduced). Since this is often a very slow back and forth process, the journey patients go through is frequently something like this as the brain tries to rewire itself:

Note: While it is not an SSRI, the notorious malarial preventative melfoquinine (Lariam) or melfoquinine has many similar side effects to the SSRIs, requires a similar adjunctive protocol to treat (e.g. no alcohol), and causes similar up and down spikes during the recovery process.
Since mefloquine’s effects are not due to withdrawals (as they are triggered by taking the drug, worsen with each successive dose and persist long after you’ve stopped it), I suspect they are instead due to it being heavily flourinated. Likewise, many believe the side effects of the SSRIs are in part due to their numerous fluorine groups (which are on many but not all SSRIs).
Amongst other things, we find fluorinated drugs tend to affect the central nervous system and are much harder for the body to eliminate (which we suspect is related to how fluorinated compounds persist in the environment).
In my previous articles on SSRIs, I hence stated that if you plan to discontinue a SSRI, you need to find a psychiatrist to help you do it. Unfortunately, since I have multiple friends who do this, I did not realize at the time how difficult it was to find someone like them. For example:
• Many of the members on survivingantidepressants.org had first unsuccessfully sought help from primary care providers and emergency rooms, and then seen multiple psychiatrists, elite clinics, and specialists such as neurologists and endocrinologists without finding anyone who could help them.
• While everyone on in that community wants knowledgeable medical providers to refer people to, no one in that community has found them.
So for that reason, I decided to extensively review this topic and compare what the surviving antidepressant community, my colleagues and I have found to be true on this subject, particularly since some of the approaches my colleagues can significantly reduce the time it takes to recover from these drugs. For those in need, the guide we created for ways to assist in safely withdrawing from SSRIs (which an immensely challenging task) can be found in the final section of this article.
Note: The article you reading now is an abridged version of the one which contains that guide.
What I find particularly interesting about this subject is how many of the approaches they’ve utilized overlap with what frequently needs to be done to heal a COVID-19 vaccine injury — which in turn speaks to how poorly equipped our conventional medical system is to deal with complex neurological illnesses.
Conclusion
It has always deeply upset and disturbed me that drugs like the SSRIs can be allowed to be on the market and I frequently think about what my life would be like if I had been one of those unfortunate people who trusted my doctor and took an SSRI.
Presently, I believe there are two major reasons why the SSRIs are so popular and have persisted despite overwhelming evidence arguing against their usage.
• First, they provide a quick and easy solution to a complex problem. Very few people want to take the time to figure out what the root of someone’s unhappiness or mental illness is (e.g., past trauma, unmet spiritual needs, an onslaught of technology separating us from nature, brain damage or a chronic inflammatory condition), so giving them the option of instead pushing a pill and being able to claim they “solved” the mental illness is the easy way out a lot of people (and governments) will take.
For example, not too long ago, I talked to a mental health social worker, who eventually shared that even though she knows the drugs aren’t good for her clients, she supported the them being used because otherwise it would be so much more work to manage her clients. I in turn shared that I understood the constraints she was under and recognized in certain cases, psychiatric medications are the correct treatment for someone.
However, I made it clear that I strongly disagree with their approach and believe the fundamental flaw in modern medicine is its belief that it is its place to dominate the human body mind and spirit as in most cases to solve a problem you instead need to support its ability to heal.
• Second, since so much money is made from selling psychiatric medications (as they can essentially be given to everyone for life at a very high mark-up) it is inevitable that corruption will ensure everything is done to ensure that market will continue to flourish and they will be sold to as many people as possible regardless of the consequences of doing so.
In essence, both of these are not that different from vaccines. Consider the promise of vaccination — they can be easily administered to a large number of people and in turn solve all the complex diseases healthcare systems struggle with (when in reality they can’t and create far more chronic ones). So, when vaccines fail to live up to their promise, the authorities respond by attributing their failure to not enough people vaccinating and pushing even more vaccines on the population.
For example, as I began to show in this article (with bipolar disorder), the advent of psychiatric medications has greatly increased rather than decreased the amount of mental illnesses in our society, but this has not caused anyone to reconsider the wisdom of this approach (e.g., consider how hostile the APA psychiatrists were to the idea their drugging might be worsening bipolar disorder).
Likewise, vaccines are also a key product for the pharmaceutical industry since they have a high markup and are guaranteed to be sold to a lot of people (especially the annual ones) once the FDA approves the vaccine (which it almost always does) and then to varying degrees, everyone else mandates it.
In the next part of this series, I will look at exactly how these dangerous drugs were pushed onto the market (since there are so many appalling parallels to what happened with the COVID-19 vaccines) and in the final part, I will look at how the depression industry was created to them to sell those pills to the world.
A Note From Dr. Mercola About the Author
A Midwestern Doctor (AMD) is a board-certified physician in the Midwest and a longtime reader of Mercola.com. I appreciate his exceptional insight on a wide range of topics and I’m grateful to share them. I also respect his desire to remain anonymous as he is still on the front lines treating patients. To find more of AMD’s work, be sure to check out The Forgotten Side of Medicine on Substack.
